Treatment for Your Child’s Single Ventricle: Stage II Surgery
|
|
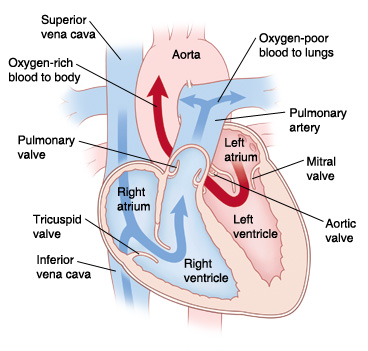
| In a normal heart, oxygen-poor blood is pumped to the lungs from the right ventricle. Oxygen-rich blood is pumped to the body from the left ventricle. |
Your child has a heart problem that is a single ventricle heart defect. This means that one of the ventricles is either too small or is absent. The most common treatment for this problem is heart surgery. This is often done in three stages. This sheet explains what is done during the second stage (stage II). The surgery cannot repair your child’s heart problem. But it can help relieve your child’s symptoms. It may also increase your child’s chances of living a more normal life. The doctor can answer your questions and tell you more as needed.
The goals of heart surgery for single ventricle heart defects
- Stage I. Make the single working ventricle the main pumping chamber of the heart, providing blood to both the lungs and the body.
- Stage II. Decrease the workload of the single ventricle, and reduce the mixing of oxygen-poor and oxygen-rich blood.
- Stage III. Separate the circulation of blood in the heart so that there is very little mixing of oxygen-rich and oxygen-poor blood.
|
What are the risks and complications?
- Infection
- Bleeding
- Problems with the nervous system, such as seizure or stroke
- Abnormal heart rhythm (arrhythmia)
- Abnormal buildup of fluid around the heart or lungs
- Problems in the lungs
- Damage to the nerves that control the vocal cords or the diaphragm
|
Stage II: The bidirectional Glenn (BDG) procedure
|
|
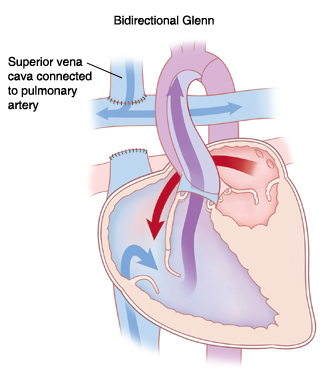
| The BDG procedure sends oxygen-poor blood returning from the upper body directly to the lungs. This helps decrease the workload of the single ventricle. |
The second stage of the surgery is called the BDG procedure. It is most often done when a child is 4 to 6 months old. A hospital stay of 5 to 7 days may be needed. The procedure provides low-pressure blood flow to the lungs. And it helps reduce the workload of the single ventricle. During the surgery, the surgeon:
- Separates the superior vena cava (SVC) from the heart. The SVC is the large blood vessel that brings oxygen-poor blood from the upper body to the right atrium. This blood vessel is cut from the right atrium. The end closest to the right atrium is closed off. The other end is sewn to the right pulmonary artery. This allows oxygen-poor blood from the upper body to flow directly to the lungs, without passing through the heart. There, it receives oxygen.
- Removes any additional source of blood flow to the pulmonary artery. If a shunt, band, or other device was placed during a previous procedure to direct blood to the lungs, it is removed at this time.
- Fixes any other abnormal structures.
|
When to call your child's healthcare provider
Call your child's healthcare provider right away if any of these occur:
- Increased redness, draining, swelling, or bleeding at the incision site
- Increased swelling of the head and neck
- Fever of 100.4°F (38°C) or higher, or as directed by your child's healthcare provider
- Trouble feeding/eating, poor appetite, or weight loss
- Shortness of breath or difficulty breathing
- Color changes (gray, pale or blue) of the skin, lips or fingernails
- Cough that won’t go away
- Increased tiredness or irritability
- Prolonged nausea or vomiting
- Irregular heartbeat
- No noticeable improvement or you don't think your child is getting better
|