Coronary Stents
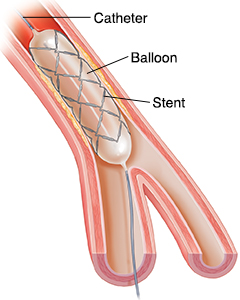
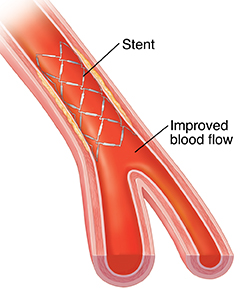
A stent is a small metal coil or mesh tube that is placed in a narrowed artery to hold it open. This helps improve blood flow to your heart. The stent also helps keep the artery from re-narrowing (restenosis). Some stents are coated and slowly release medicine over a time. This reduces the amount of scar tissue that forms in the artery, helping prevent restenosis. A heart specialist called an interventional cardiologist does coronary angioplasty and stenting. He or she has specialized training in using the equipment and in doing the procedure as safely as possible.
 |
 |
During the procedure
-
A member of your healthcare team will numb the skin at the insertion site with a local anesthetic. This is usually the groin or the wrist) with a local anesthetic. He or she will make a needle puncture to insert the catheter.
-
Your doctor will insert a guide wire through the thin, flexible tube (catheter) and move it to the narrow spot in your heart's artery. Your doctor tracks its movement using pulsed X-ray called fluoroscopy. An angiogram will be done which is an X-ray movie of heart artery blood flow using contrast. This identifies the location of the stenosis.
-
Your doctor will then insert a balloon-tipped catheter through the guide catheter and thread it over the guide wire. He or she will position it at the narrow part of the artery.
-
Your doctor will deliver a stent mounted on a balloon-tipped catheter to the blockage in your artery.
-
He or she will inflate the balloon to expand the stent.
-
The expanded stent further compresses the plaque against the artery wall, increasing the blood flow to the heart muscle.
After the procedure
-
Your doctor will give you medicine to prevent blood clots from forming on the new stent. You will continue to take this medicine until the stent and artery have healed. Your healthcare team will tell you how long you should take this. Your doctor will give you a prescription before you go home. This prescription is often for a medicine called clopidogrel. This medicine is usually taken with aspirin to prevent blood clots from forming inside of the newly opened area of the artery which would cause a heart attack.
-
Your healthcare team will tell you how long to lie down and keep the insertion site still. The amount of time may depend on whether a closure device such as a stitch or collagen plug was used to close the opening made in your artery. The time you must be still may be shorter if one of these devices was used. The amount of time will also depend on if there is any bleeding at the artery site.
-
If the insertion site was in your groin, you may need to lie down with your leg still for several hours. A pressure band is often used to hold pressure on the wrist. It's slowly removed once there is no sign of bleeding.
-
A nurse will check your blood pressure and the insertion site.
-
You may be asked to drink fluid to help flush the contrast liquid out of your system.
-
You will likely be given other prescriptions to prevent other areas of the arteries from narrowing. This includes medicine to control cholesterol, such as statins. You may also get a beta blocker to prevent a heart attack. Nitroglycerin is prescribed to treat episodes of chest pain (angina) if this occurs. Don't mix nitroglycerin with medicines that are used to treat erectile dysfunction or pulmonary hypertension. This can cause a dangerous drop in your blood pressure.
-
You need to have a follow up appointments to check how well you respond to the stent and new medicines. This can be as early as a week or maybe within 2 to 4 weeks of your coronary stent.
-
You may stay for several hours overnight in the hospital. Have someone drive you home from the hospital.
-
It’s normal to find a small bruise or lump at the insertion site. This should disappear within a few weeks.
-
You will be given discharge instructions that tell you how to keep the puncture site clean and dry and what activity restrictions you may have after your procedure. Make sure you ask your healthcare team about any questions or concerns you have after your procedure.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Angina (a feeling of pain, pressure, aching, tingling, or burning in the chest, back, neck, throat, jaw, arms, or shoulders)
-
Increasing pain, swelling, redness, bleeding, or drainage at the insertion site
-
Severe pain, coldness, or a bluish color in the leg or arm that held the catheter
-
Shortness of breath
-
Trouble urinating or blood in your urine
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider